nutrition
The Best Vitamins And Supplements For Bone Health
On This Page

Calcium is an essential component to healthy bones and the earlier you start taking it, the better. Build up your reserves today to maintain healthy bones..
Why Bone Health is Important
When it comes to health and wellness, the skeletal system is truly an unsung hero. All too often, bone health doesn’t receive the attention it deserves until later in people’s lives — often after the opportunity to support long-term bone health foundation has passed.
Your bones give your body shape, produce red blood cells, store crucial minerals, protect vital organs, and enable the movement of work and play. But far from being a static structure, bones are dynamic and are constantly producing hormones to signal bone breakdown and regeneration. Understanding and supporting this process is important for maintaining a high quality of life as you age.
We’ll discuss the most important vitamins and minerals for bone health and how you can incorporate each of them into your daily routine.
Calcium
As you probably know, calcium makes up a significant portion of your bones and teeth. Calcium is actually the most abundant mineral in the body, and well-known for its importance to bone health. Adequate calcium intake is one of the most important factors in building a strong skeletal system. Among its bone-supporting functions, calcium also aids in muscle contraction, blood clotting, and signaling between cells.
A tall, calcium-packed glass of milk is iconic for its bone benefits. In addition to dairy, other significant sources of calcium include leafy greens, like kale and spinach, as well as small bone-in fish like sardines, soybeans, broccoli, and okra.
Not eating these foods too often? Fortunately, many cereals, breads and juices are fortified with calcium. Additionally, calcium supplements can also increase your intake and help avoid a potential deficiency. It is recommended that women consume 1,000-1,200 mg of calcium per day through a combination of food and, if needed, supplements.
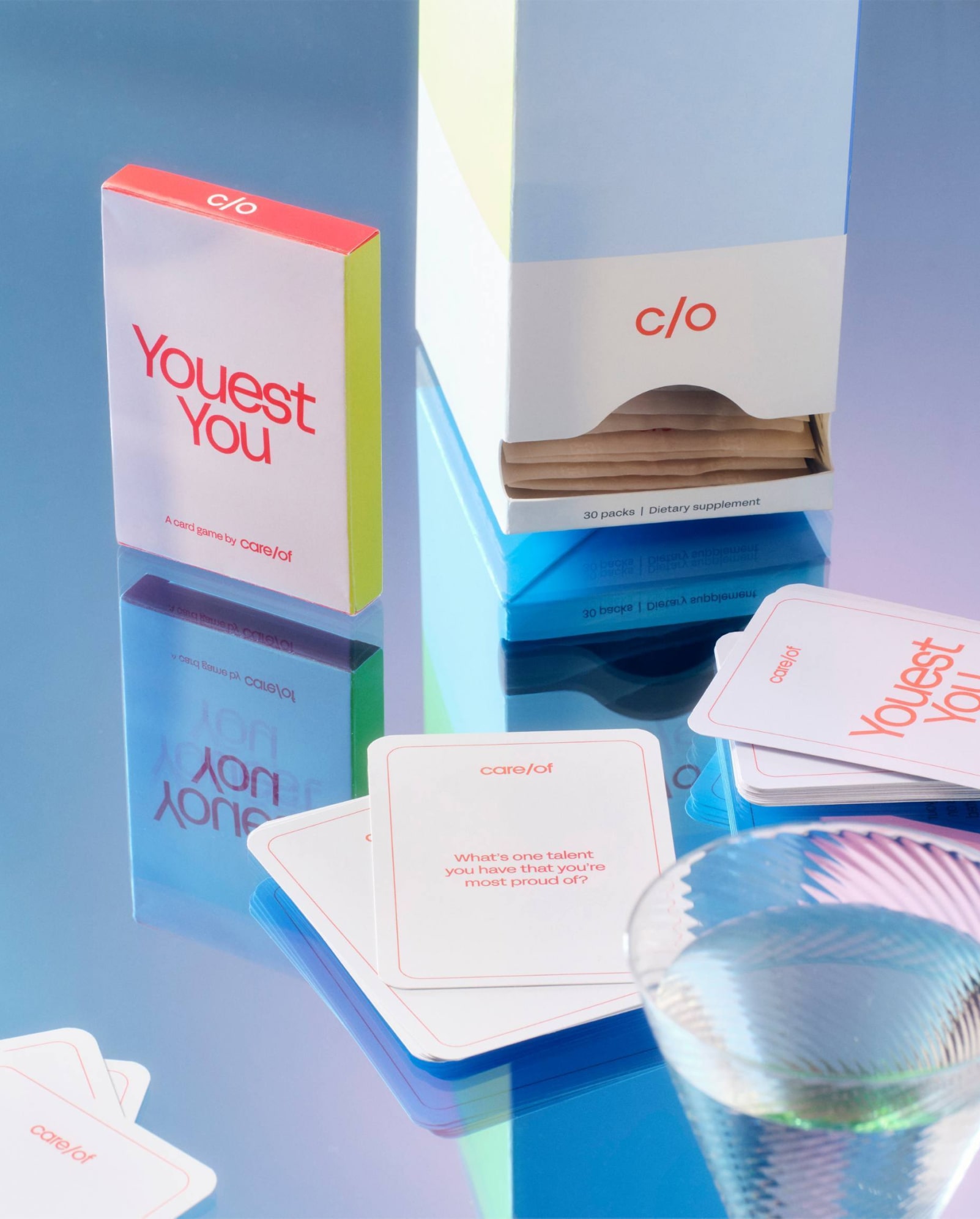
Care/of’s Calcium Plus supplement provides not only calcium but also vitamin D, magnesium, and vitamin K2 which all work synergistically with calcium to support proper bone health.
Though proper intake of calcium is essential, its dosage does have an Upper Limit (UL). Going past this limit can cause potential digestive discomfort. For adults ages 19 to 50 years old, the UL for calcium intake is 2,500 mg, and for those 51 and over, the UL is 2,000 mg.
Most people hit the point of peak bone mass between the ages of 25-30, and a slow age related decline can happen beginning around age 40.
Ideally, calcium intake should be sufficient during youth and young adulthood to lay down as much bone mass as possible. So if you’re in this stage of life, consider intentionally meeting your daily calcium intake needs. In addition to age, alcohol and smoking can cause calcium depletion. Post-menopause also presents a time when bone health may take a hit due to natural decrease in estrogen, a key hormone that helps regulate bone mass and metabolism.
Regardless of your age, know that you can still positively impact your bone health! Good nutrition and regular exercise can help to promote optimal bone health.
Factors that influence calcium intake and bone density
For most people, calcium intake will be one of the most important minerals in managing bone health. However, other factors should be taken into consideration: gender, age, ethnicity, and family history all influence your unique needs.
Certain medical conditions, absorption issues, certain types of restrictive diets, and medications can influence your body’s ability to utilize calcium properly.
Sudden changes or imbalances in hormone production can negatively impact bone health. It is widely known that menopause can contribute to bone density issues, as the body’s production of estrogen diminishes. Similarly, men with low testosterone levels may experience changes in bone density. Similarly, an imbalance of thyroid hormones can also contribute to bone density challenges.
Of course, there are the usual culprits as well: heavy alcohol use, smoking, and excessive caffeine consumption all interfere with calcium intake, and thus, bone health.
Vitamin D
Vitamin D is calcium’s trusted companion. Emerging science has shown that vitamin D allows calcium to be sufficiently absorbed in the gut and used by the body.
In addition to supporting the absorption of calcium, vitamin D also aids in bone growth and remodeling. A 2010 study showed that the combination of vitamin D and calcium did effectively support bone health.
Vitamin D does not occur naturally in many foods. The best source of vitamin D is through direct sun exposure during the brightest part of the day. Of course, not everyone is fortunate enough to reside in a region where this is possible year round. For this reason, supplementation is often recommended. The recommended dose range for ages 9 through 70 is between 600 and 4,000 IU per day, or about 15-100 mcg.
Vitamin K
Vitamin K is a fat-soluble vitamin that plays a role with bone proteins, regulating genes that impact osteoblasts (cells that build bone) and bone resorption (breakdown of bone for use in the body). In addition to bone health, vitamin K is also essential for blood clotting and wound healing and is involved in a protein that may be able to promote vascular health.
There are two main types of vitamin K– K1 and K2. Vitamin K1 (phylloquinone) is the main dietary source of vitamin K found mostly in green leafy vegetables. Vitamin K2 (multiple types of menaquinones) is mainly produced by gut bacteria but is also present in small amounts in animal-based foods and fermented foods like natto.
While the body can convert some vitamin K1 into K2, the process is inefficient. Instead, the best ways to improve vitamin K2 levels include increasing intake of vitamin K2 rich foods, supporting gut health through intake of a variety of plant foods and probiotics, and supplementation. Newer research shows that vitamin K2 supplementation can improve regulation of blood glucose levels (already in normal range) through mediation of the gut microbiome, particularly increases in short-chain fatty acids in the gut.
Vitamin C
Vitamin C is a water-soluble vitamin perhaps best known for its role in supporting immune function. This vitamin acts as an antioxidant to help manage oxidative stress which can disrupt many aspects of health when not kept in check.
In addition to immune health, vitamin C is also required in collagen formation, protein metabolism, and formation of some neurotransmitters.
Vitamin C’s antioxidant properties help to manage the oxidative stress that can impair collagen formation. Collagen is the main protein network that makes up connective tissues including bones. The body also needs adequate levels of vitamin C to enable absorption of nonheme iron, the type of iron in plant-based foods.
Those with a heightened risk for lower levels of vitamin C include people who smoke, have digestive and absorption issues, and don’t eat enough fruits and vegetables containing vitamin C.
Foods rich in vitamin C include peppers, broccoli, citrus fruits, Brussels sprouts, kiwi, strawberries, and papaya. Care/of’s Vitamin C supplement contains vitamin C from acerola cherries and as well as the helpful bioflavonoids often present in vitamin C rich foods to support absorption and utilization in the body.
Magnesium
Magnesium is the unsung hero of bone health. An essential mineral required in over 40% of all processes in the body, magnesium also aids the body in regulating calcium levels. Approximately 50-60% of the body’s magnesium is stored in the skeletal system. Due to its importance in bones, both structurally and functionally, it cannot be left out of any discussion of bone health.
Like vitamin D, magnesium supports calcium’s functions. Specifically, it is active in the transport of calcium across cell membranes. Additionally, it supports the structural development of new bone tissue.
Magnesium is plentiful in nuts, seeds, dark leafy green vegetables, tuna, and beans. If you aren’t regularly eating these foods, consider a magnesium supplement, especially if you consume alcohol or caffeine, which both deplete magnesium levels in the body.
Foods That Help With Bone Health
To support strong and healthy bones, eat foods rich in the vitamins and minerals that we’ve discussed so far that aid in the structure and functioning of bones.
Yogurt and cheese
Dairy products are generally rich in calcium. One cup of plain whole milk yogurt contains about 311 mg of calcium, which is about 25-30% of adult daily calcium needs. Fermented dairy products such as yogurt, kefir, and ripened hard cheeses also contain vitamin K2 which aid in bone health.
Green Vegetables
Green leafy vegetables, such as spinach, kale, collard greens, and broccoli are rich in vitamin K. Spinach, kale and collard greens are particularly rich in calcium and vitamin C, with kale providing over 100% of the RDA for vitamin C in just 2 cups raw. Spinach comes out on top among these vegetables for being rich in magnesium.
Fish
Fish are nutrient powerhouses. They have a good mix of vitamins and minerals that promote healthy bones. Fatty fish is also rich in omega-3 fatty acids, which play a crucial role in bone density and strength and maintaining healthy blood vessels. Fish is also a good source of vitamin D, which is not naturally occurring in many foods. Fish with small bones still retained for consumption, such as sardines, anchovies, and salmon, are also a great source of calcium. Eating the skin on fish is also an excellent way to up your intake of collagen to support the health of bones and other connective tissues.
Beans
Beans are rich minerals like calcium, magnesium, and phosphorus which all contribute to strong bones. Soybeans, black beans, and lima beans are particularly good sources of magnesium.
Lifestyle Factors for Bone Health
In addition to eating enough foods that contain bone-supportive nutrients, other aspects of lifestyle and nutrition play a major role in bone health.
Exercise
Regular physical activity is one of the key modifiable risk factors that can positively impact bone health, as it helps to maintain bone density and strengthand offers anti-aging benefits. During adolescence and young adulthood when bone mass capacity can still be increased, weight-bearing exercise is essential to draw closer to peak bone mass. Weight-bearing exercise should be part of one’s regular routine in order to maintain current bone mass and increase the strength of bones.
Eat a balanced diet
Eating a balanced diet can help ensure you get enough of the vitamins and minerals we’ve discussed so far that support bone health. Beyond these particular nutrients, other aspects of a healthy diet includes eating antioxidant-rich foods. Foods rich in antioxidants can help to combat the oxidative stress that can disrupt collagen formation in bones and other connective tissues and negatively impact bone mass.
The Bottom Line
Building and maintaining healthy bones is important regardless of your age or gender. It is never too early to prepare for natural age related changes in bone density. Many factors influence your bone health, but one important aspect to focus on is getting the vitamins and minerals your body needs to feel strong at every age.
Because your bones are made up of calcium, calcium is of the utmost importance in your health routine. Recent studies show that consuming vitamin D alongside magnesium and vitamin K2, in addition to calcium, is the ticket for healthy bones. If you decide to supplement, make sure the doses, particularly of calcium and vitamin D, don’t go overboard.
To determine if supplementation is necessary based on your lifestyle and other risk factors, you can take an online lifestyle assessment. Feel the difference in your bones.